Treatment for shingles?
The severity and duration of an attack of shingles can be significantly reduced by immediate treatment with antiviral drugs, such as acyclovir, famciclovir, or valacyclovir, which can reduce the duration and pain of shingles.
Over-the-counter pain medicines may be prescribed to, such as acetaminophen, to help reduce pain.
Topical antibiotics may be prescribed to limit infection of the blisters.
Resources
|
Side effects > Side effects of the skin
Last update: 09/11/2014
|
TOPICS
Skin Rashes | Itching (Pruritus) | Shingles | Quick Reference
Research News | Skin cancers (melanoma)
In the News
Rashes and dry skin are common occurrences for patients receiving chemo or radiation therapy. They can be alarming to the patient, but will often resolve after a time.
 TOPIC SEARCH PubMed TOPIC SEARCH PubMed
NOTE: Rashes can result as a side effect of some treatments, be a symptom of lymphoma, or be unrelated to the disease or treatment. Skin Rashes and Other Changes The location, appearance and color of a rash will help your doctor make the diagnosis. Look for care suggestions on this chart for common rashes.
Common causes of rashes include:
Allergies to medications may present as skin rashes. Note: "Allergic reactions produce an array of symptoms that affect the skin, airways, and heart -- usually within an hour of exposure." [1] Allergic reactions can be serious and life threatening in some cases.
Skin infections. Depressed immunity - a common side effect of many cancer treatments - can also predispose you to skin infections such as cellulites, or reactivation of dormant viral infections such as Herpes Zoster (Shingles).
Lymphomas affecting skin Lymphomas can originate or spread to the skin. See Extranodal > Cutaneous (B cell and T cell Lymphomas. The later provides images, but it should be noted that only a biopsy can diagnose a lymphoma with certainty.
Itching (pruritus):
 Is the sensation of itch) can result from some kinds of lymphoma, or from conditions secondary to the lymphoma and treatments - but there are many other causes. Is the sensation of itch) can result from some kinds of lymphoma, or from conditions secondary to the lymphoma and treatments - but there are many other causes.
Chronic pruritus (itching) is associated with reduced quality of life. Poor sleep patterns, anxiety and depression are common, and may worsen the itch.
 TOPIC SEARCH PubMed TOPIC SEARCH PubMed
In the News:
.gif) |
Now@NEJM blog: Chronic Pruritus
http://blogs.nejm.org/now/index.php/chronic-pruritus/2013/04/26/
|
Treatment of chronic pruritus should be directed at the underlying cause when possible. The presence of skin findings may be caused by scratching which can camouflage causes of the itch. In some cases. Cutaneous-barrier insufficiency is common and made worse by repetitive scratching, which exposes skin to irritants.
Chronic pruritus can be caused by the following disorders
Cutaneous (dermatologic / skin) disorders:
atopic eczema,
psoriasis,
ichen planus,
scabies
Systemic causes:
cholestasis (a condition where bile cannot flow from the liver to the duodenum)
chronic kidney disease
hyperthyroidism
lymphoma, (particularly Hodgkin and cutaneous t-cell lymphoma)
myeloproliferative disorders
Neuropathic causes:
notalgia paresthetica (distinctive itch of upper back)
brachioradial pruritus (characteristic itch of the arms, probably caused by
spinal-nerve pinching)
Psychogenic causes:
stemming from emotional or mental stresses
Certain drugs:
such as opioid analgesics
Undetermined origin - when the underlying cause is unclear
Treatments:
As always a medical professional should be consulted to identify the likely cause and the most appropriate approach to treatment.
This list is provided to aid in the questions you might ask of your doctor. The approach to treatment will depends on the underlying cause, such as treating the lymphoma or hyperthyroidism - but only if these conditions are the cause for the itch.
.gif) |
Topical emollients for mild or localized itch and for xerosis (winter itch)
|
.gif) |
“Wet pajama” treatment can be helpful and soothing when extensive inflammation is present, as in severe atopic dermatitis (discuss with doctor)
|
.gif) |
Capsaicin, which acts locally by desensitizing peripheral-nerve fibers
|
.gif) |
Topical anesthetics
|
.gif) |
Topical menthol
|
.gif) |
Topical glucocorticoids
|
.gif) |
Systemic (oral drug) antihistamines
|
.gif) |
Neuroactive Medications,
such as Gabapentin and pregabalin
|
.gif) |
Antidepressants or selective serotonin-reuptake inhibitors
|
.gif) |
Opiate agonists and antagonists
|
.gif) |
Phototherapy
|
.gif) |
Search of: pruritus clinical trials- ClinicalTrials.gov http://1.usa.gov/13cE9XZ
Adapted from NEJM: Clinical Practice - Chronic Pruritus
http://www.nejm.org/doi/full/10.1056/NEJMcp1208814
|
Resources:
.gif) |
Pruritus - overview and risk factors cancer.gov/ meb.uni-bonn.de/cancer.gov
|
.gif) |
Pruritus and Systemic Disease emedicine.medscape.com
|
.gif) |
Evaluation of pruritus online.epocrates.com
|
.gif) |
Pruritus and Systemic Disease: Treatment & Medication emedicine.medscape.com |
Return to top
Shingles
Frequently asked Question: Is a Shingles vaccine safe for me?
"Up to one in ten older patients won't be candidates for the vaccine because of weakened
immune systems due to cancer therapy, organ transplants, HIV/AIDS, or other causes.
The vaccine contains live but weakened varicella virus that could overwhelm the immune systems of those patients. Source: WebMD
 What is shingles? "Shingles (herpes zoster) is an outbreak of rash or blisters on the skin that is caused by the same virus that causes chickenpox — the varicella-zoster virus. What is shingles? "Shingles (herpes zoster) is an outbreak of rash or blisters on the skin that is caused by the same virus that causes chickenpox — the varicella-zoster virus.
The first sign of shingles is often burning or tingling pain, or sometimes numbness or itch, in one particular location on only one side of the body. After several days or a week, a rash of fluid-filled blisters, similar to chickenpox, appears in one area on one side of the body.
Shingles pain can be mild or intense. Some people have mostly itching; some feel pain from the gentlest touch or breeze. The most common location for shingles is a band, called a dermatome, spanning one side of the trunk around the waistline. Anyone who has had chickenpox is at risk for shingles.
Scientists think that in the original battle with the varicella-zoster virus, some of the virus particles leave the skin blisters and move into the nervous system. When the varicella-zoster virus reactivates, the virus moves back down the long nerve fibers that extend from the sensory cell bodies to the skin. The viruses multiply, the tell-tale rash erupts, and the person now has shingles." ninds.nih.gov
It's very important to recognize and treat shingles early to limit the severity of the infection. See Patient education for self-referral and on-demand treatment for herpes zoster in lymphoma patients. Leuk Lymphoma. 1993 Nov;11(5-6):447-52. PMID: 8124217 and related abstracts
Common sites for shingles
(click to enlarge image on http://hcd2.bupa.co.uk )
The nerve roots that supply sensation to your skin run in pathways on each side of your body. When the virus becomes reactivated, it travels up the nerve roots to the band-like area of skin supplied by those specific nerve roots.
Shingles develops in stages:
| Prodromal stage (before the rash appears) |
| - |
Headache, sensitivity to light |
| - |
Flu-like symptoms (chills, stomach ache, diarrhea) without a fever - may develop just before or along with the start of the rash. |
| - |
Itching, tingling, tickling, numbness or extreme pain in the area around the affected nerves several days before a rash begins. |
|
Active stage (rash and blisters appear)
|
| - |
belt-shaped or band-like rash - the clearest sign of shingles. |
| - |
The rash appears on only one side of your body, usually the chest or back, and sometimes on your face around one eye, which may threaten your sight unless you receive prompt treatment. |
| - |
A rash consisting of small fluid-filled blisters develops on reddened skin
on one side of your body. |
| - |
Fluid inside the blister is initially clear but may become cloudy after 3 to 4 days. |
| - |
The rash caused by shingles is more painful than itchy. |
| - |
The discomfort occurs on a single side of the body, commonly on the chest
or back, but it may occur on the abdomen, head, face, neck, or one arm or leg. |
adapted from WebMD
|
.gif) |
Shingles: Herpes Zoster WebMD | BUPAS | ninds.nih.gov
.gif) |
Management of Herpes Zoster (Shingles) and Postherpetic Neuralgia aafp.org
|
.gif) |
Shingles: An Unwelcome Encore By Evelyn Zamula FDA
|
|
.gif) |
Allergic Reactions
.gif) |
Elimination Diet and Food Challenge Test WebMD
|
.gif) |
Allergy-Proof Your Environment WebMD
|
|
.gif) |
Common Skin Infections: Cellulitis, Erysipelas, Impetigo pdrhealth
|
.gif) |
Skin Rashes and Other Changes The location, appearance and color of a rash will help
your doctor make the diagnosis. Look for care suggestions on this chart for common rashes.
|
.gif) |
Shingles immunization? WebMD
"Up to one in ten older patients won't be candidates for the vaccine because of weakened
immune systems due to cancer therapy, organ transplants, HIV/AIDS, or other causes.
The vaccine contains live but weakened varicella virus that could overwhelm the immune
systems of those patients.
|
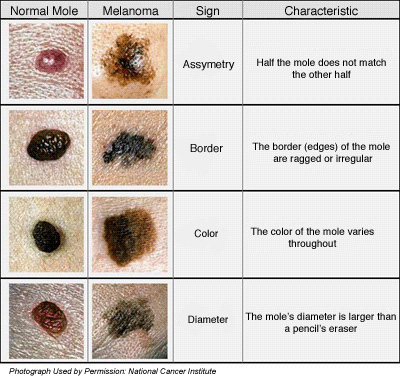
Skin cancers occur more frequently in lymphoma survivors
could be secondary to treatment or a risk factor of the disease
Action: Be sure to self-check for suspicious moles (see chart below), and have your doctor examine you regularly - once a year.
See also: An association between cutaneous melanoma and non-Hodgkin's lymphoma: pooled analysis of published data with a review oxfordjournals
"Chronic immune suppression is suggested as a risk factor for the development of both cutaneous melanoma and non-Hodgkin's lymphoma. The increased risk of cutaneous melanoma after non-Hodgkin's lymphoma could arise from immunodeficiency as a result of the disease itself or the drugs used to treat it. Cytotoxic chemotherapy has an immunosuppressive effect and could explain the increased risk of a subsequent cutaneous melanoma among patients with non-Hodgkin's lymphoma treated with chemotherapy"
Asymmetry: half of the mole does not match the other half
Border: the border (edges) of the mole are ragged or irregular
Color: the color of the mole varies throughout
Diameter: moles with a diameter larger than a pencil's eraser
Evolving: changing in shape and size in short period of time.
See also: What Does Melanoma Look Like? - National Cancer Institute http://1.usa.gov/1eEnAHw
Alert from Carol: "Any lesion that grows rapidly should be checked by a dermatologist immediately? Non-pigmented melanoma is literally that--it looks like skin."
Related resource:
.gif) |
Lymphoma survivors are at a higher risk for this dangerous skin cancer.
The following compares normal to abnormal moles as you advance each slide.
* The ABCDEs of Moles and Melanomas | Cancer Network http://bit.ly/1BuK0rz
|
|