TOPICS
Putting Risks in Perspective | Resources - General | Stem Cell | Treatment-Related Mortality | Cardiac Toxicity | Immune Suppression | Myelodysplasia & AML- Leukemia | Secondary Cancers ... Melanomas | Transformation
 TOPIC SEARCH: PubMed: Doxorubicin AND cardiac toxicity | Purine analogs AND immune suppression | Auto SCT and secondary cancers TOPIC SEARCH: PubMed: Doxorubicin AND cardiac toxicity | Purine analogs AND immune suppression | Auto SCT and secondary cancers
Also see Side Effects | About Transformation
 Here we will post abstracts and resources that describe some of the more serious risks associated with cancer therapies, primarily: secondary cancers, myelodysplastic syndrome, and long-term immune suppression. Here we will post abstracts and resources that describe some of the more serious risks associated with cancer therapies, primarily: secondary cancers, myelodysplastic syndrome, and long-term immune suppression.
But we will also try to put the risks into perspective by noting how likely they are to manifest, and in how much time; and by balancing the risks of treatment against the dangers of delaying or avoiding appropriate treatments.
For example, while it's true that alkylating agents (such as Leukeran and Cyclophosphamide) increase the risk of developing secondary cancers, the increased risks appear to be relatively small and minimal compared to letting the disease progress unchecked. Importantly the risks can often take many years to emerge, often as long as 10 to 20 years.
See Related PubMed abstracts & Abstracts on Second Malignancies - Medscape free login req.
Alkylating agents, radiotherapy, autologous transplants, and splenectomy increase the risk of developing MDS (Myelodysplastic Syndrome - failure of the bone marrow to produce healthy and sufficient blood cells), but the risks of developing MDS range from small to significant ( 3 - 12%) depending on the therapy type (Auto Transplant seems to have the highest risk), but this approach is generally tried when the patient has aggressive and/or refractory disease.
Some treatments may be associated with the transformation of indolent lymphomas to a more aggressive disease. However, be aware that associations between specific treatment and transformation do not prove that one caused the other, because transformation is also a part of the natural course of the disease.
See About Transformation
It appears to be especially prudent to carefully assess treatment-related risks when the treatment path is unclear, as is often the case for indolent lymphomas.
Resources - General
.gif) |
Defining and Assessing Quality Cancer Care, - www.nap.edu - PDF
|
.gif) |
Evaluating medical claims and data
for additional information about the limitations of information provided in
abstracts and various types of studies.
|
Collecting Stem Cells following treatment
-
MCP Chemotherapy Regimen May Reduce Amount of Stem Cells Collected in Follicular Lymphoma - cancerconsultants.com
"According to results recently published in Annals of Oncology, the chemotherapy regimen consisting of melphalan, chlorambucil, and prednisone (MCP) appears to interfere with the ability to collect enough stem cells for an autologous stem cell transplant in patients with follicular non-Hodgkin’s lymphoma.
Treatment-related Mortality
-
Treatment related mortality: Cytochrome P450 2C19 loss-of-function polymorphism is associated with an increased treatment-related mortality in patients undergoing allogeneic transplantation. Bone Marrow Transplant. 2007 Oct;40(7):659-64. Epub 2007 Aug 6. PMID: 17680025
Comment: Probably this finding needs to be validated (reproduced by an independent group) before being declared as true, but it shows how normal variations in patients (a polymorphism) can affect outcomes. In this case, treatment-related mortality is strongly correlated with a specific normal genetic variation
Cardiac Toxicity
Immune suppression - Infectious Complications
Almost all treatments for lymphomas suppress or impair immunity. The degree of immune suppression depends on many factors, including dose, dose timing, and the type of agent. Some agents are associated with more significant immune suppression than others. In general, younger patients are better able to recover bone marrow function following treatment than the elderly.
"Fludarabine use in previously treated patients with CLL may be associated with infections involving T-cell dysfunction, such as listeriosis, pneumocystosis, mycobacterial infections, and opportunistic fungal and viral infections. These infections may result from T-cell depletion secondary to fludarabine use. Prophylaxis or presumptive therapy should be initiated when appropriate.
Treatment with alemtuzumab, a monoclonal antibody, affects both B cells and T cells and shows a pattern of infections similar to that of purine analogs. Varicella zoster virus, herpes simplex virus, and CMV are all common in patients with CLL." Source: medscape.com (free login req.)
Related Articles:
.gif) |
A new model for predicting infectious complications during fludarabine-based combination chemotherapy among patients with indolent lymphoid malignancies. Cancer. 2004 Nov 1;101(9):2042-9. PMID: 15372472
|
.gif) |
Warning label added to Rituxan -
the label was "revised to indicate that hepatitis B virus reactivation with fulminant hepatitis, hepatic failure and death has been reported in some patients with hematologic malignancies who were treated with Rituxan since its approval." - pharmexec.com Oct 2004
|
.gif) |
Rituximab treatment results in impaired secondary humoral immune responsiveness.
Blood. 2002 Sep 15;100(6):2257-9. PMID: 12200395 | Related articles
|
.gif) |
Infectious complications associated with purine analogs (such as fludarabine) - Related abstracts
|
.gif) |
Impact of therapy With chlorambucil, fludarabine, or fludarabine plus chlorambucil on infections in patients with chronic lymphocytic leukemia: Intergroup Study Cancer and Leukemia Group B 9011.
J Clin Oncol. 2001 Aug 15;19(16):3611-21. PMID: 11504743 - PubMed
|
Myelodysplasia (MDS) & Leukemias
Also See Side Effects > Myelodysplastic Syndrome
A "rare and potentially fatal blood disorders that occur when the body starts incorrectly manufacturing the three types of blood cells - white, red, and platelets - resulting in malformed, immature cells." See - Myelodysplasia Syndromes, Basic Explanations PDF
The following "Published data suggest that the risk of treatment-related-AML/ and treatment-related MDS following standard chemotherapy is 1% to 1.5% per year from 2-10 years after initiation of therapy."
Leukemogenic therapies are agents that increase the risk of developing leukemias. - "The risk of leukemia was greatest four or five years after chemotherapy began, and the risk was elevated for at least eight years after the cessation of chemotherapy. The drugs cyclophosphamide, chlorambucil, melphalan, thiotepa, and treosulfan were independently associated with significantly increased risks of leukemia, as was the combination of doxorubicin hydrochloride and cisplatin. Chlorambucil and melphalan were the most leukemogenic drugs, followed by thiotepa; cyclophosphamide and treosulfan were the weakest leukemogens, and the effect per gram was substantially lower at high doses than at lower doses. The extent to which the relative risks of leukemia are offset by differences in chemotherapeutic effectiveness is not known." nejm.org
.gif) |
NEW Secondary malignancies after therapy of indolent NHL
Haematologica 2008 93: 336-338., Jonathan W. Friedberg - full text haematologica.org
Second malignancies have clearly evolved to be important causes of morbidity and mortality in patients with indolent lymphomas. As survival times increase, and the cohort of patients treated with modalities such as purine analogs, aggressive autologous transplantation and novel radioimmunotherapy grows, it can be expected that the incidence of second cancers will increase significantly. Perhaps most concerning is the lack of an apparent plateau in the incidence curve, even 20–30 years after diagnosis of lymphoma. For this reason, it is critical that patients in prolonged remission remain under care of medical and radiation oncologists attuned to these risks, and undergo at least annual evaluation (history and physical examinations), with appropriate screening tests for second cancers. In the future, emphasis must continue to be given to minimizing toxic therapy to prevent this devastating cost of cure.26 Finally, it is important to realize that the risk of MDS/AML associated with radioimmunotherapy may not be substantially different from the risk in patients treated with standard chemotherapy, including both alkylating agents and purine analogs.
|
.gif) |
RIT and risk of MDS: Treatment-related myelodysplastic syndrome (MDS) and AML in patients treated with Zevalin radioimmunotherapy. J Clin Oncol. 2007 Sep 20;25(27):4285-92. Epub 2007 Aug 20.
PMID: 17709799
Analysis of data from patients ... (746 patients) ... incidences of t-MDS and t-AML (0.7% per year after treatment) are consistent with that expected in patients with NHL who have had extensive previous chemotherapy treatment and do not appear to be increased after treatment with the ibritumomab tiuxetan regimen.
|
.gif) |
Myelodysplasia and acute myeloid leukemia following therapy for indolent lymphoma with fludarabine, mitoxantrone, and dexamethasone (FND) plus rituximab and interferon alpha - bloodjournal.org full
|
.gif) |
Specific Regimen [FND] Influences Risk of Myelodysplasia After Lymphoma Treatment - Medscape (free login req.) or ASCO
|
.gif) |
Armitage JO, Carbone PP, Connors JM, et al. Treatment-related myelodysplasia and
acute leukemia in non-Hodgkin's lymphoma patients. J Clin Oncol. 2003;21:897-906. Abstract
|
.gif) |
Secondary myelodysplasia following purine analog therapy - Abstract No: 2477
|
.gif) |
Therapy-related myeloid leukemias are observed in patients with chronic lymphocytic leukemia after treatment with fludarabine and chlorambucil: results of an intergroup study, cancer and leukemia group B 9011. J Clin Oncol. 2002 Sep 15;20(18):3878-84. PMID: 12228208 - PubMed
|
.gif) |
Treatment-Related Myelodysplasia and Acute Leukemia in Non-Hodgkin's Lymphoma Patients. J Clin Oncol. 2003 Mar 1;21(5):897-906. PMID: 12610191 - PubMed | Full text
|
Secondary Cancers in Lymphoma Survivors
 TOPIC SEARCH: PubMed TOPIC SEARCH: PubMed
.gif) |
* JCO, 2010:
Second Malignant Neoplasms in Survivors of Pediatric Hodgkin's Lymphoma Treated With Low-Dose Radiation and Chemotherapy http://bit.ly/1m33v6f
Cumulative incidence of first second malignant neoplasms (SMN) was 17% (95% CI, 10.5 to 26.7) at 20 years after HL diagnosis. The standard incidence ratio (SIR*) for any second malignancy was 22.9 (95% CI, 14.2 to 35) with an absolute excess risk of 93.7 cases per 10,000 person-years.
Standard Incidence ratio (SIR): "The expected number is calculated by multiplying each age-specific cancer incidence rate of the reference population by each age-specific population of the community in question and then adding up the results. If the observed number of cancer cases equals the expected number, the SIR is 1. If more cases are observed than expected, the SIR is greater than 1. If fewer cases are observed than expected, the SIR is less than 1. www.state.nj.us
|
.gif) |
Secondary malignancies after therapy of indolent non-Hodgkin’s lymphoma
Jonathan W. Friedberg haematologica.org/
The true incidence of MDS/AML and other secondary malignancies after treatment for indolent lymphoma, outside of the setting of autologous transplantation, is largely unknown. Historical series have suggested that the incidence of secondary malignancies is almost double the expected incidence over a 10-year follow-up period and patients treated with total body irradiation have an even higher risk.13–15
|
.gif) |
Secondary Malignancies: What, When, Why, in Whom? - Smita Bhatia, MD, MPH
NCCN Clinical Practice Oncology Forum. 2008; ©2008 NCCN Clinical Practice Oncology Forum
Posted 10/27/2008
The growing population of cancer survivors carries a significant burden of morbidity, necessitating comprehensive long-term follow-up, which should ideally begin at the completion of active therapy.
Documentation of therapeutic exposures will form the basis for use of recommendations within the long-term follow-up guidelines, thus ensuring standardization of care received by the survivors. However, many barriers prevent effective follow-up, the most fundamental of which are the lack of understanding by long-term survivors about their risk, as well as by the primary care physicians caring for them.
Shortcomings of the healthcare system are also potential barriers to long-term follow-up, and include infrastructure issues, such as a lack of capacity within centers, training and educational deficiencies, and inadequate/ineffective communication between oncologists and primary care physicians who subsequently provide the large bulk of follow-up care.
|
.gif) |
Risk factors for development of a second lymphoid malignancy in patients with CLL.
Br J Haematol. 2007 Nov;139(3):398-404. PMID: 17910629
|
.gif) |
The risk of secondary malignancies over 30 years after the treatment of non-Hodgkin lymphoma.
Cancer. 2006 May 17; PMID: 16708354 | Related articles
.gif) |
Cancer risk higher in lymphoma survivors - reuters.com
"Survivors had an 8.8-fold increased risk of leukemia and a 1.6-fold risk of lung cancer, according to the report in the Journal of Clinical Oncology"
|
|
.gif) |
Risk of Second Malignancy After Non-Hodgkin's Lymphoma: A British Cohort Study.
J Clin Oncol. 2006 Mar 6; [Epub ahead of print] PMID: 16520465 | Related articles
|
.gif) |
Researchers Learn More About Secondary Cancers After Non-Hodgkin's Lymphoma - cancerconsultants.com
|
.gif) |
Second cancers among long-term survivors of non-Hodgkin's lymphoma.
J Natl Cancer Inst. 1993 Dec 1;85(23):1932-7. PMID: 8230284
|
.gif) |
Risk of leukemia following treatment for non-Hodgkin's lymphoma - jncicancerspectrum.oxfordjournals.org/
"Our results suggest that prednimustine may be a human carcinogen, with a positive dose-response gradient evident for ANLL risk. The low, nonsignificant risk of leukemia associated with cyclophosphamide was reassuring because this drug is commonly used today. Despite the excesses of ANLL associated with specific therapies, secondary leukemia remains a rare occurrence following NHL. Of 10,000 NHL patients treated for 6 months with selected regimens including low cumulative doses of cyclophosphamide and followed for 10 years, an excess of four leukemias might be expected."
|
.gif) |
AAOS: Increased Rate of Secondary Cancers Seen in Long-Term Osteosarcoma Survivors - pslgroup.com
|
.gif) |
MEDLINE Abstracts: Second Malignancies from Medscape Hematology-Oncology
What's new about therapy-related malignancies in cancer patients? - Medscape free login req.
|
.gif) |
New malignancies after blood or marrow stem-cell transplantation in children and adults: incidence and risk factors. J Clin Oncol. 2003 Apr 1;21(7):1352-8. Erratum in: J Clin Oncol. 2003 Aug 15;21(16):3181.
PMID: 12663726 | Abstracts
|
.gif) |
Researchers Learn More About Secondary Cancers After Non-Hodgkin’s Lymphoma - cancerconsultants.com
" Researchers concluded that secondary cancers after NHL are often treatment-related, but other sources, such as immune suppression and environmental exposures, may also play a role in the development of secondary cancers and malignancies."
|
.gif) |
Second cancers and late toxicities after treatment of aggressive non-Hodgkin lymphoma - bloodjournal.org
|
Melanomas
It is prudent to check for melanoma often if you have lymphoma.
-
Study Connects Melanoma And Non-Hodgkin's Lymphoma - Cancer 2001; 91:874-880
-
Melanoma Images
-
Visible Warning Signs (ABCDE's):
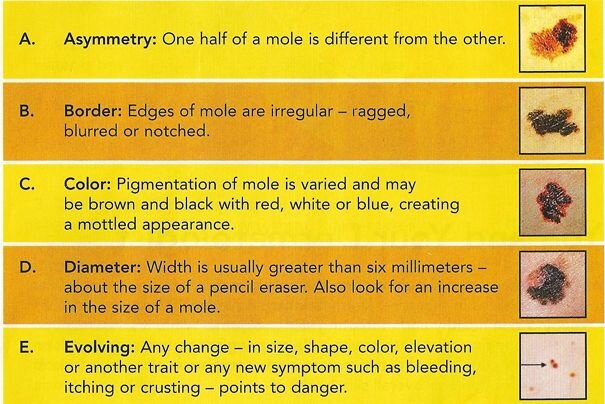
If you have any of the above features - or anything else out of the ordinary - show your doctor as soon as possible.
Source: RITE AID pharmacy
Transformation
See About transformation
.gif) |
|
.gif) |
Large-cell transformation of chronic lymphocytic leukemia and follicular lymphoma during or soon after treatment with fludarabine-rituximab-containing regimens: natural history- or therapy-related complication? Eur J Haematol. 2002 Feb;68(2):80-3. PMID: 12038452 - PubMed
|
|