|
Tests & Imaging > About CT Imaging
Last Updated: 08/19/2014
|
TOPICS
Intro | ACR accreditation | What to Expect and How to Prepare | About Long-term Risks of CT PET/CT | Resources and Research News
 Computed Tomography (CT) is an imaging procedure commonly used to determine locations and sizes of tumors, so-called staging of disease. CT is often used to measure response to treatment, especially in clinical trials. Computed Tomography (CT) is an imaging procedure commonly used to determine locations and sizes of tumors, so-called staging of disease. CT is often used to measure response to treatment, especially in clinical trials.
X-ray images are taken from different angles and then processed by a computer to create detailed pictures of the inside of the body. Each section of the test involves lying still for about 10-30 minutes. The images produced are in cross sections.
|
Search for ACR accredited Diagnostic Imaging Centers
ACR accreditation means: "Your hospital, clinic or health center has voluntarily gone through a rigorous review process to be sure it meets nationally accepted standards. The personnel are well qualified, through education and certification, to perform and interpret your medical images and administer your radiation therapy treatments. The equipment is appropriate for the test or treatment you will receive, and the facility meets or exceeds quality assurance and safety guidelines."
Accredited Facility Search - American College of Radiology http://bit.ly/1pY8d4i
FDA resource on Computed Tomography (CT) http://1.usa.gov/10a43Kn
Use this handy record to track your imaging history
My Medical Imaging History -- from imagewisely.org: http://bit.ly/1tiwFPc
Before undergoing any X-ray exam or treatment procedure, remember to ask your doctor:
• Why do I need this exam?
• How will having this exam improve my health care?
• Are there alternatives that do not use radiation and which are equally as good?
Remember:
• Be sure to tell the doctor or technologist if you are, or might be, pregnant
before having an exam.
• Don’t insist on an imaging exam if the doctor explains there is no need for it.
• And, don’t refuse an imaging exam if there’s a clear need for it and the clinical benefit outweighs the small radiation risk.
For more information, go to www.ImageWisely.org and www.fda.gov/ForConsumers/ConsumerUpdates/ucm095505.htm
|
What to expect and how to prepare
.gif) |
Bring water with you so that you can drink after the test to more quickly eliminate the contrast material.
|
.gif) |
Depending on the area to be scanned, you may be asked not to eat for approximately 4-6 hours prior to the test.
|
.gif) |
Depending on the scan, IV contrast may be used.
|
.gif) |
The technologist begins by positioning the patient on the CT table. You may be given pillows to help hold still and in the proper position during the scan. A wedge is usually available (ask the tech) for under the knees to help support the back. The table will move slowly into the CT scanner.
|
.gif) |
Drink water after the test
|
.gif) |
Ask for copies of the images |
Patient-to-patient advice: "When you have these scans, remember to ask the technician for copies of the films (for your records). They don't mind printing an extra CD or print - as long as you tell them upfront BEFORE they sent the "number of copies". Everything is digitalized and it makes it so much easier to keep your records. In the olden days, we would have the big, heavy CT films or MRI films we carried around. So, the improvements are welcomed, however, I have also learned that computers crash and some digital films get lost, hence, my recommendation that you ask for copies. If you are nervous about asking for this, call them before you go and find out if you can bring a CD for them to back up to. In this way, you will learn if your facility is co-operative or not. And naturally, always ask for a copy of the radiology report to be mailed to your home for your records.
Having CTs spaced on different days is very, very common. Personally, I had to have them several days apart because I am very sensitive to the contrast dye. I also have to be pre-medicated with Benadryl and Prednisone. It is one of the reasons that I "gave up" CTs for monitoring remission. You don't have this type of control while in a clinical trial and you must comply with the demands of the trial protocol. Those of us who have already participated in a trial understand how confusing it can be when they request something of you and you don't understand the why of it.
One way that you might look at the four areas of scan is "insurance" - while it is not necessary to have, it is good backup against unseen or undiagnosed areas of disease involvement. Also, a head/neck scan now, if clear, will be your baseline for the future. Hopefully, you will never have evidence of disease from the neck up, but if you should have questions, you could refer back to those scans.
One of my patients has a little "thumb" drive (USB 2.0 flash driver) or other named device she carries with her for her scans. The local imaging center copies her scans onto her zip/flash driver and she has it to go back to her home computer. I was with her when she had her physician's appointment (who didn't have the "films" yet) so Linda just popped her little flash drive into his laptop and up came her scans. It worked out so well, but I think it depends on your facility and their "spirit of cooperation". Some imaging centers act like they are guarding the secrets of the universe and YOU are not allowed to know the secrets of the universe because you don't wear a white jacket!!! "You must ask your doctor!!" ~ Jama Beasley (advisor to PAL, and patient navigator)
Factors that can influence interpretation of results
.gif) |
Size of lymph nodes can be influenced by inflammatory reactive conditions.
"diffuse lymph node enlargement secondary to infectious or granulomatous diseases cannot be discriminated from metastases or systemic lymphoma." Oncologic Imaging: A Dilemma Still Waiting to Be Solved
|
.gif) |
Scar tissue - CT cannot distinguish between scar tissue and viable tumors.
Following treatment "a residual mass persisting on CT after treatment poses a common clinical dilemma: it may indicate the presence of viable lymphoma, which requires further treatment, or it can be benign, consisting of only fibrotic and necrotic tissues." PMID: 12644887 For this reason PET or Gallium scans may be used after treatment to help differentiate active disease from scar tissue.
|
.gif) |
Small changes in the size of nodes could be accounted for by the angle of the equipment in relation to the patient.
"In a multiplanar reconstruction CT program (CT/MPR), the altered gantry angle corresponding to the patient's position during scanning for multiplanar reformatted CT may cause distortion of the image. The aim of this study was to quantitatively assess the distortion in reformatted central panoramic and cross-sectional images owing to the change of gantry angle. " birjournals.org
|
Recommended Resources
.gif) |
About CT imaging Cancer Help. Org | radiologyinfo.org
|
.gif) |
|
PET/CT
"The highly sensitive PET scan detects the metabolic signal of actively growing cancer cells in the body and the CT scan provides a detailed picture of the internal anatomy that reveals the location, size and shape of abnormal cancerous growths.
Alone, each imaging test has particular benefits and limitations but when the results of PET and CT scans are "fused" together, the combined image provides complete information on cancer location and metabolism.
The bottom line is that you can have both scans - PET and CT - done at the same time." petscaninfo.com
.gif) |
PET/CT Imaging radiologyinfo.org
|
Also See
.gif) |
Comparing CT and MR Images Lymphomation.org
Side-by-side comparison of MR and CT images
|
.gif) |
Comparing CT with MRI Lymphomation.org
Abstracts and resources on the subject.
|
|
|
About Long Term Risks of CT Imaging
First, it's important to note that cautions about risks of a secondary cancer from CT is generally aimed at the general public and in particular younger people who may receive CT imaging without a clear cut medical necessity to do so.
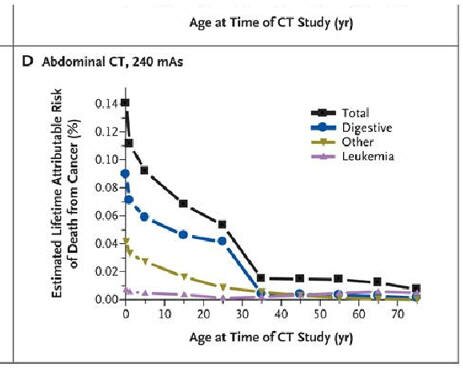
The following graph illustrates that the risk from a single CT is not insignificant - but that it decreases substantially with age.
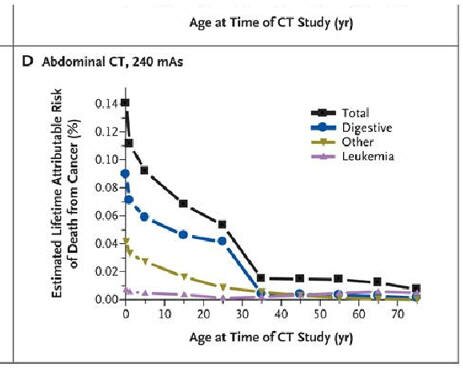
Source: Computed Tomography — An Increasing Source of Radiation Exposure,
N Engl J Med 2007; 357:2277-2284
* Multi Media Presentations on Radiation Protection &
Radiation Safety Training 
Excellent explanation of dosing, effective dose, etc., with animations.
Expert commentary on CT risks
by Orhan H Suleiman MS, Ph D, FAAPM:
.gif) |
Age is a significant factor ...
"Radiation effects are latent, not showing up until many years later.
They are also considered stochastic, that is a term used by the radiological community which really means probabilistic. They will never occur for most individuals, but although the risk is not "zero", it effectively is for most individuals." 1
"Many cancers show up 5, 10, and 50 years later (as the atomic bomb survivors are showing). Leukemia and thyroid cancers show up within a few years, and usually drop off. It varies for different cancers. Also, the older you are, the more likely you will die of something else.
|
.gif) |
It is prudent to carefully plan such imaging studies so that only the necessary information is collected, and that the amount of radiation the patient receives is, in fact, as low as reasonably achievable, the ALARA principle (As Low As Reasonably Achievable)." 1
|
.gif) |
Radiation dose from imaging diagnostics and treatment is cumulative ...
... but low dose radiation is not equivalent to high exposure (ie, an h-bombs) because the body apparently adjusts and heals when doses are divided up for treatments - known because so called fractionated doses can be given in higher cumulative doses as treatment.
|
.gif) |
Treatment doses are higher than diagnostic, and the effective dose is finely tuned and well documented in therapeutic radiation.
"Secondary cancers associated with radiation therapy are more probable, since these radiation doses are thousands, or tens of thousands greater than the radiation doses associated with imaging. 1
|
.gif) |
Diagnostic x-rays use low dose ionizing radiation, but dosing is less precise, more variable.
|
.gif) |
Different organs have different sensitivities to ionizing radiation. Marrow, breasts, gonads, etc. (Marrow is sensitive).
|
.gif) |
Dose terminology (Rem, Gray, mSv, ...) has confounded even the experts and makes comparing exposures very difficult ...
... but now we have so-called effective dose (E), which allows for easier comparisons of exposures and risks . The measure of effective dose is mSv. ( Effective dose in millisieverts (mSv).)
Some examples of E:
= Natural Environmental background in 1 year ~ 3 mSv
= Chest x-ray ~ to .02 mSv (2.4 days of natural environmental radiation (NER))
= CT abdomen ~10 mSv (3.3 years of NER)
(~ means approximately equal to)
The current occupational cumulative regulatory limits are
.gif) |
Individual worker in general population
1 mSv , or 50 chest xrays, or 4 months NER
|
.gif) |
Worker
50 mSv, or 2500 chest xrays, or 16.7 yrs NER
|
.gif) |
Emergency worker
500 mSv, or 25,000 chest xrays, or 167 yrs NER
The relative dose of radiation from CT is much larger than other imaging tests, but the risks are still very small that CT imaging will lead to a secondary cancer.
|
|
.gif) |
However, the risks from many CT images is not insignificant, particularly if you are young and require frequent monitoring.
Some factors that influence risk
.gif) |
The lower doses in diagnostic imaging *reduces* the risk of secondary cancers (compared to high exposures (h-bombs etc)) by 2-3 times.
|
.gif) |
Radiation risk is age dependent
= Adolescents and young adult have ~ 2-3 times greater cancer risk per unit dose,
= Adults over 50 have ~ 1/4th the relative risk per unit dose*
Most lymphoma patients are over 50.
|
.gif) |
The radiation dose in medical imaging can vary by as much as 100 times
Some factors
= patient size (being larger increases the E)
= equipment design, operator settings, length of exam ...
= amount of radiopharmaceutical administered
|
|
.gif) |
How to minimize your risk?
.gif) |
Keep records of all x-ray exposures so you can give objective information to your doctor about your cumulative dose.
|
.gif) |
Ask for a breast shield. See Breast Shield Cuts CT Scan Radiation www.realage.com
|
.gif) |
Inform your doctor about regulatory limits for ionizing radiation, and your current estimated effective dose.
|
.gif) |
Ask the imaging providers to give information about the *effective dose* in mSv that you will receive.
... And if the ALARA principle is followed at the center (As low as Reasonably achievable)
|
.gif) |
Ask the imaging center to see their ACR (American College of Radiology) accreditation.
|
.gif) |
Ask your doctor if your clinical situations allows for imaging at longer intervals.
|
.gif) |
Ask if MRI can be used instead of CT, particularly if you are young and if your past exposure has been high. New ACR accredited MRI can do a good job of staging lymphomas. Both CT and MRI have strengths and weaknesses depending on the area of the body being looked at.
|
.gif) |
Clinical trials: Trials can sometimes require patients to get imaging done more often and a closer intervals (as short as 2 months) When making your case to the investigator about using MRI instead of CT, provide the background facts in summary form, and include your estimated cumulative effective dose. Inform the investigator that the FDA probably considers ACR accredited MRI images equivalent to CT.
|
1 Expert commentary by Orhan H Suleiman MS, Ph D, FAAPM
|
Further reading:
It's not easy to quantify the risk: Comparisons of CT exposures with exposures to background radiation received in air travel may be useful. According to the FDA: One pelvic CT is roughly equivalent to exposures to cosmic radiation from 333 flights from Los Angeles to New York and back (.03 mSv) (Radiation Safety).
A twenty-year career as a member of a flight crew might add up to roughly: 300 days x 20 years, or 6,000 days of exposure to cosmic radiation. Dividing this number by 333 gives us a very rough equivalent of 18 pelvic CT scans (10 mSv).
Note that despite the increased exposure, the study found "No consistent association between employment period or duration and cancer mortality was observed." Mortality from cancer and other causes among male airline cockpit crew in Europe.
..." key factor in the body's response to ionizing radiation is the relative sensitivity to radiation of the various cell types that comprise body tissues. Bergonié and Tribondeau's Law (1906) implies that rapidly dividing cells (e.g., cells of the blood forming tissues and certain groups of immature sperm cells) are among the most sensitive to acute effects of radiation. The more highly differentiated cells (e.g., muscle and nerve cells) are less vulnerable to acute injury by radiation.
Other factors that influence the expression of the deterministic effects of radiation include the region of the body irradiated and variation between individuals in their physiologic response to radiation." http://books.nap.edu
.gif) |
QUESTION: Is it true that PET/CT involves decreased radiation exposure compared to a stand-alone CT? Doesn't sound logical to me, but it's something I've heard from several places.
Andy (on WebMagic) writes:
"It does seem logical that a PET/CT should have the radiation due to a PET plus the radiation due to a CT and therefore more than a CT.
But CT's are complicated things and the amount of radiation depends on how close together they make the slices (or how tight the spiral is since they don't really do slices anymore) and how much resolution is desired. Basically, the more detail they want the more radiation is used.
On the other hand, newer scanners get more detail for a given amount of radiation than some of the older ones. So, the radiation from a CT scan is very variable.
The CT scan done during a PET/CT is generally gives a less detailed image than those done for CT scans by themselves. I think this is because in a PET/CT the CT part is largely so they can identify what part of the body is giving off the higher SUV values while in a CT scan the goal is enough detail to give the sizes and shapes of each lymph node, organ, ... Taken together this allows a PET/CT to have a lower total radiation dose than a regular CT (if there is such a thing). Really, if you want to worry about the various doses it is best to check them at the imaging center where you get scanned.
Personally, I am glad that my onc tends to scan less [for indolent follicular lymphoma] and so I know that when she does it that the benefits outweigh the risks. On the other hand, I am willing to undergo more scans in a clinical trial if I think the benefit of the trial warrants the extra risk (which is probably small). I don't monitor all of my radiation but just want to know that each time I am scanned that there is a good reason and that some action may well be taken based on the results."
On the dose of radiation, an advisor commented:
"It may be unethical to expose patients to too high a radiation dose, but do consider that it might be just as unethical to expose them to a dose that was significant yet not quite high enough to obtain really useful images."
|
.gif) |
NPR Walt Bogdanich interview:
[Benefits and] Hidden Dangers Of Medical Radiation 
Includes many useful tips - questions to ask, who to ask, how to identify credentialed centers ....
|
.gif) |
Dec 19, 2009: Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. - ncbi.nlm.nih.gov
|
Results Radiation doses varied significantly between the different types of CT studies. The overall median effective doses ranged from 2 millisieverts (mSv) for a routine head CT scan to 31 mSv for a multiphase abdomen and pelvis CT scan. Within each type of CT study, effective dose varied significantly within and across institutions, with a mean 13-fold variation between the highest and lowest dose for each study type. The estimated number of CT scans that will lead to the development of a cancer varied widely depending on the specific type of CT examination and the patient's age and sex.
An estimated 1 in 270 women who underwent CT coronary angiography at age 40 years will develop cancer from that CT scan (1 in 600 men), compared with an estimated 1 in 8100 women who had a routine head CT scan at the same age (1 in 11 080 men). For 20-year-old patients, the risks were approximately doubled, and for 60-year-old patients, they were approximately 50% lower.
Related articles
.gif) |
Resources on Imaging Safety, including Contrast PAL
|
.gif) |
Radiation Exposure of Patients Undergoing Whole-Body Dual-Modality 18F-FDG
PET/CT Examinations jnm.snmjournals.org
|
.gif) |
What are the Radiation Risks from CT? FDA
|
.gif) |
Breast Shield Cuts CT Scan Radiation www.realage.com
|
.gif) |
Radiation Biology By: Scott Williams, MD auntminnie.com
Comprehensive review of risks ... "it is reasonable to assume that certain factors can modify the ultimate effects of radiation [3]. Factors such as age at time of exposure and the manner in which the radiation was received can affect the risk relationship."
|
.gif) |
Mortality from cancer and other causes among male airline cockpit crew in Europe.
Int J Cancer. 2003 Oct 10;106(6):946-52. PMID: 12918075
|
.gif) |
Radiation Safety radiologyinfo.org
|
.gif) |
Maintaining a Proper Perspective of Risk Associated with Radiation Exposure PDF
Michael A. Thompson, Division of Medical Imaging and Therapy, University of Alabama at Birmingham, Birmingham, Alabama
|
.gif) |
Radiation Risk From CT Scans: A Call for Patient-Focused Imaging ~ Richard C. Semelka, MD
Medscape Radiology 6(1), 2005. © 2005 Medscape
Richard Semelka, MD, is one of the preeminent practitioners of abdominal MRI in the United States and is a frequent contributor to Medscape Radiology.
The hot-button issues raised in this opinion piece call into question some of the current practices surrounding the use of CT scanning. It's the opinion of this editor that a topic of importance, such as the safety and health of patients referred for diagnostic imaging evaluation, merits a broad dialogue in an open, spontaneous, and timely forum.
full text Medscape (free login req.)
|
.gif) |
Doctors' knowledge of radiation exposure: questionnaire study, 2003 BMJ
Conclusion: "Overall, 97% of the answers were underestimates of the actual dose; six (5%) doctors did not realize that ultrasound does not use ionising radiation; and 11 (8%) did not realize that magnetic resonance imaging does not use ionizing radiation."
|
.gif) |
How many CTs are too many? Lymphomation.org
"In order to make truly informed decisions, it's important to put the risks of procedures into context and not to magnify them."
|
.gif) |
Radiation Dose Comparisons FDA
|
.gif) |
Radiation doses in computed tomography - The increasing doses of radiation need to be controlled BMJ 2000;320:593-594 (4 March)
|
.gif) |
Radiation dose in [CT] scans could be halved BMJ 2001;323:185 (28 July)
|
.gif) |
Second malignancy after treatment of childhood non-Hodgkin lymphoma. Cancer. 2001 Oct 1;92(7):1959-66. PMID: 11745271 PubMed Provides clues about long-term risks.
|
.gif) |
|
|
|